Medicaid at a Glance
VIRGINIA MEDICAID OVERVIEW
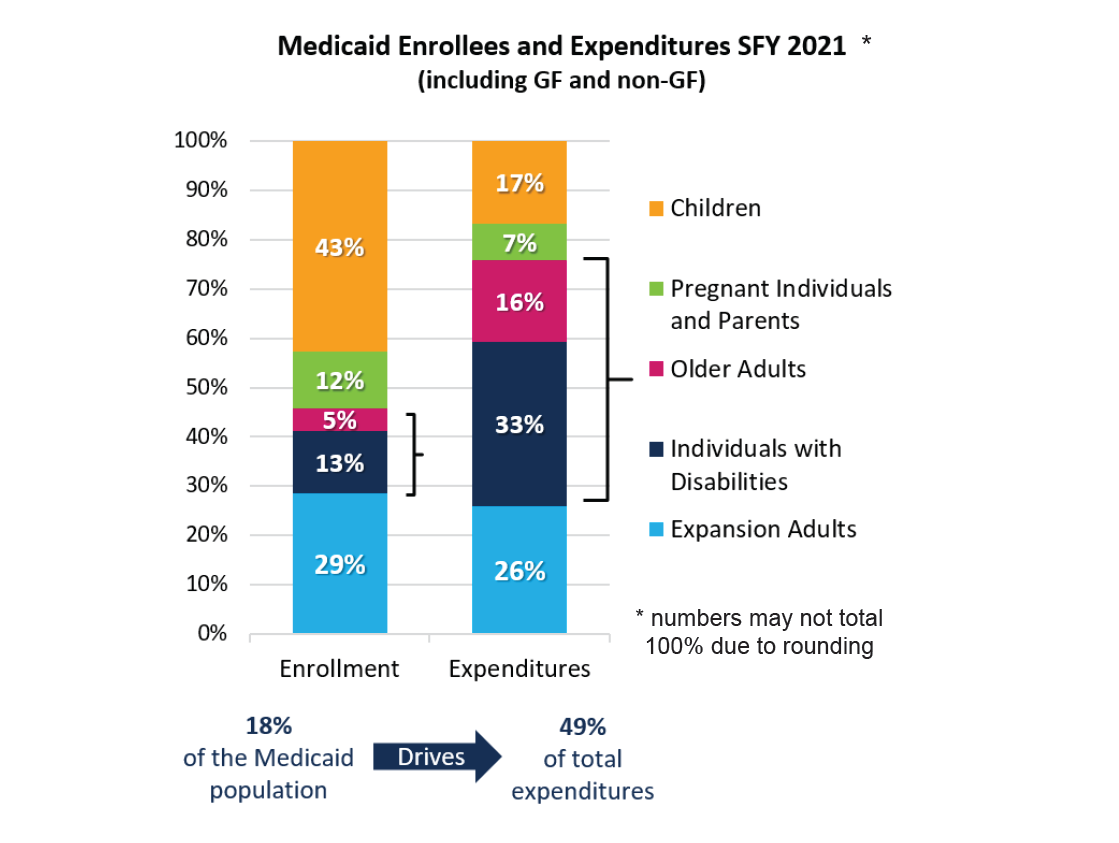
The Virginia Department of Medical Assistance Services (DMAS) plays an essential role in the Commonwealth’s health care system by offering lifesaving coverage to one in five Virginians. Children are the largest eligibility group served by Virginia Medicaid, with more than 800,000 members. Other eligible populations include people with disabilities, older and low-income adults, and pregnant individuals.
For more than two decades, the Virginia Medicaid agency has provided health coverage through a successful managed care model that now serves more than 96% of full-benefit Medicaid members, who can choose from six managed care health plans available statewide.
NEW BEHAVIORAL HEALTH SERVICES
Virginia Medicaid members have access to nine new behavioral health services launched in 2021 that strengthen crisis response and address a national emergency in mental health care for youth. These new services help members avoid hospital stays through access to preventive, community-based options. The services are part of a collaboration with the Virginia Department of Behavioral Health and Developmental Services through a multi-phase initiative known as Project BRAVO (Behavioral Health Redesign for Access, Value and Outcomes).
The new behavioral health services include:
- Mobile crisis response teams
- Short-term crisis supports
- 23 hours of observation
- Short-term intervention services
- Partial hospitalization during daytime hours
- Intense outpatient therapy and counseling a few times a week
- Community-based team supports for adults experiencing serious mental illness
Check out our new Behavioral Health Service Utilization and Expenditures dashboard on the Virginia Medicaid agency website.

ADULT DENTAL BENEFIT
More than 900,000 adult Medicaid members obtained access to comprehensive dental services on July 1, 2021. The new benefit attracted bipartisan support in the General Assembly. Dental providers and health care advocates collaborated to build enthusiasm for the initiative by emphasizing the importance of oral health to achieve excellent overall health.
Adult members currently eligible for comprehensive Medicaid benefits now have coverage for dental services modeled after the benefit for pregnant Medicaid members. More than 100,000 adult Medicaid members received dental services in six months after the new benefit launched.

12-MONTH POSTPARTUM COVERAGE
Virginia is one of the first states to obtain federal approval for a measure ensuring that Medicaid members have health coverage for 12 months following pregnancy. Currently, some Medicaid members lose access to care 60 days after the end of a pregnancy. The expanded coverage, starting in 2022, will enable new parents to receive critical postpartum care, an important step in improving health outcomes for both parents and babies.
Virginia Medicaid covers one in three births in the Commonwealth. The new policy will extend coverage for more than 6,000 members annually.
MANAGED CARE QUALITY MEASURES
The Virginia Medicaid agency website has a new tool that allows members, providers and other stakeholders to track quality performance measures for our managed care program.
You can view the managed care dashboard on the Virginia Medicaid agency website.
The dashboard highlights quality measures and outcomes for seven categories in the Healthcare Effectiveness Data and Information Set (HEDIS), including access and availability of care; behavioral health services; care for children and adolescents; and substance use and monitoring.
HEDIS is a nationally recognized tool used by more than 90% of health insurance plans to measure quality of care and services. We are excited to offer this new dashboard demonstrating the value of managed care for the Virginia Medicaid program.
 Virginia Medicaid
Virginia Medicaid