Medicaid at a Glance
VIRGINIA MEDICAID OVERVIEW
The Virginia Department of Medical Assistance Services (DMAS) plays an essential role in the Commonwealth’s health care system by offering health care coverage to more than one in five Virginians through our Medicaid program, known as Cardinal Care. Cardinal Care covers over 2 million Virginians; the largest populations being low-income adults and children. Other groups covered include people with disabilities, older adults, and pregnant women.
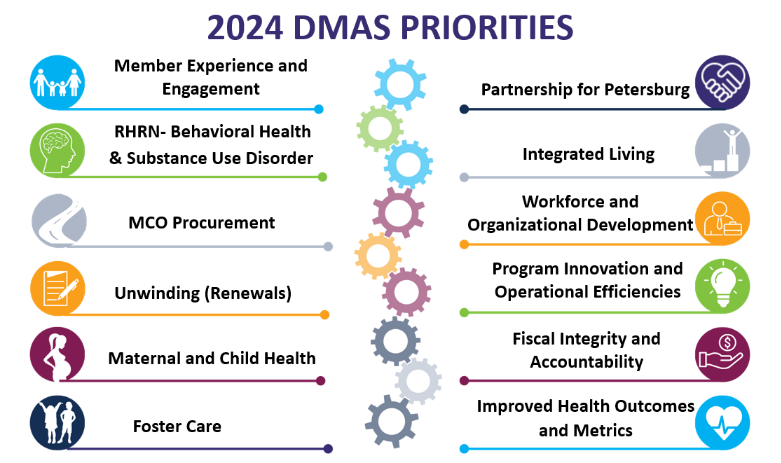
This document highlights key priorities for 2024.
Cardinal Care Managed Care – For more than two decades health care coverage is provided through managed care organizations. The managed care model provides coverage to more than 96% of members. DMAS released a request for proposals to reprocure the managed care system on August 31, 2023, for a regional implementation starting in fall 2024. For this large-scale, competitive procurement, DMAS has taken a strategic approach that prioritizes financial accountability, access to high-quality care, and support for targeted populations, including behavioral and maternal health and members in the child welfare system.
“Right Help, Right Now” Behavioral Health Transformation – Governor Youngkin created Right Help Right Now to reform the current behavioral health system in Virginia and support individuals in crisis. The goal of Right Help Right Now is to ensure an aligned approach to behavioral health that provides access to timely and effective community-based care that provides support for mental health needs, developmental disabilities, and substance use disorders on Virginians and their families. Cardinal Care plays a key role in the initiative by supporting the Governor’s Behavioral Health Transformation goals for members. This transformation includes developing new, evidence-based services and then to prepare for a request for a new 1115 waiver authority to better support members with serious mental illness (SMI). DMAS is working to provide more effective, accessible services to members and is seeking opportunities to use managed care contracts to identify and implement innovations and best practices. Some examples include outcome-based payment, performance incentives, and a focus on targeted collaboration with sister gencies, health plans, and community partners.
Maternal and Child Health – Governor Youngkin’s Administration and DMAS are revitalizing Virginia’s focus on improving maternal and child health. This includes driving improvements in both prenatal and postpartum care across all communities. The key priorities are to engage with providers and members, support maternal health in rural areas, and extend clinic hours. Through these shared goals with providers, we will work to ensure quality care is available to members. DMAS is also enhancing maternal and child health standards through the re-procurement of the Cardinal Care Managed Care Program.
Supporting Individuals with Developmental Disabilities – A key priority of Right Help Right Now is to provide needed services to more Virginians with developmental disabilities. Virginia’s Developmental Disabilities Waiver program currently provides a variety of supports with medical care, employment, community living, behavioral interventions, and other services that support employment. Increasing the number of waiver slots available will help achieve the Right Help Right Now goals and enable more members to receive life-changing services and supports in their community.
Coverage and Enrollment – DMAS, in collaboration with the Virginia Department of Social Services (VDSS) and Local Departments of Social Services (LDSS), is working to complete the renewal process for all 2.1 million Medicaid members whose redeterminations were paused during the COVID-19 Public Health Emergency. Virginia has ranked high among states during this process due to the Commonwealth’s thoughtful approach to ensuring individuals who remained eligible for coverage stayed enrolled and assisting those who were no longer eligible to transition to other coverage. DMAS has been applauded by federal partners during this process for clear and consistent member outreach and communication, as well as efforts to increase automation and update eligibility and enrollment systems. Virginia expects the redetermination of the entire Medicaid population to be completed in state fiscal year 2024, with all members resuming the regular annual review process.
Population Health – In collaboration with the Medicaid Managed Care Organizations (MCOs), DMAS has renewed its focus on community-level support. The Governor’s Partnership for Petersburg initiative will be used as a model to guide the wide-spread deployment of similar efforts across the Commonwealth. In Petersburg, DMAS and the MCOs conducted over 240 community events to promote health behaviors and drive improvement in maternal health. DMAS will work with the MCOs to advance specific interventions and targeted investments to address health-related social needs (HRSNs), as well as to strengthen partnerships between community-based organizations and health care entities. The primary focus of the work will be on addressing housing stability and food insecurity for members.
Operational Improvements and Innovations – DMAS continues to enhance its internal operations to better serve members and be accountable stewards of the taxpayer dollars that provide health care for those members. In 2024, DMAS will initiate several internal operation improvements, including the reprocurement of the core IT system that manages claims, payments, and member data. Key continuity operations, such as the automation of essential business functions, will be streamlined to ensure the DMAS workforce has the tools they need to provide services to members. DMAS remains dedicated to ensuring every employee feels safe, supported, valued, and has the tools necessary to be successful in their positions. DMAS is creating a strong workforce by attracting, developing, training, and retaining qualified employees. In 2024, DMAS has also committed to enhancing communication with members, providers, and external stakeholders through coordinated and accessible websites, digital platforms, and innovative communication strategies to keep everyone informed about the Medicaid program.
Fiscal Integrity and Accountability – DMAS continues to make fiscal accountability a top priority, to ensure the agency maintains excellent stewardship over the $23 billion in public funds that support Medicaid members. DMAS will work to ensure a fourth consecutive clean annual financial audit without any questioned costs or material findings. DMAS will also be working to ensure a fifth consecutive year without federally questioned costs that require repayment of funds. DMAS is also working to strengthen its operations in the area of lien recoveries, to ensure that Medicaid members who may have been in a car accident or had another personal injury can expeditiously settle their claims and DMAS can recoup the necessary medical expenses from those settlements. DMAS is also working to build on its work with MCOs, hospitals, nursing facilities, and other critical providers to implement accurate, timely, and transparent rate setting processes.
 Virginia Medicaid
Virginia Medicaid